Lily never planned on becoming addicted to oxycodone. Instead, she’d planned on running a marathon. But her life took an unexpected turn when she tripped during a morning jog and injured her knee. The pain was intense, and her doctor prescribed oxycodone to manage that pain.
Unfortunately, the oxycodone wasn’t enough to control Lily’s agony. She took more than the recommended dosage several times, just to take the edge off. And even though she told herself she had nothing to worry about, Lily really liked the feelings of euphoria the drug provided. She couldn’t run anymore, so she was feeling depressed. She secretly welcomed the opioid high.
Oxycodone Addiction and Opioid Detox
Lily started taking more oxycodone pills – and she took them with increasing frequency. She needed more of the drug in order to make her feel the desired high. Then one day, she ran out of pills.
That’s when Lily got sick.
Her muscles cramped up, she had a headache, she felt nauseated, and she was sweating profusely. She searched her symptoms online and quickly realized she had become physically dependent on the opioid painkiller.
The steady supply of opioids was no longer there, and her body’s systems were reacting with a fierceness in the drug’s absence. Lily understood in that moment she experiencing oxycodone withdrawal.
Symptoms of Oxycodone Withdrawal
Some of the typical symptoms people experience when they quit oxycodone include:1
- Muscle cramps
- Vomiting and nausea
- Diarrhea
- Cold and hot flashes
- Anxiety
- Trouble sleeping
- Sweating
- Headache
- Watery eyes and nose
Note: It is possible to become physically dependent on oxycodone when you take it as prescribed. Your body gets used to the presence of the drug, so when you stop taking oxycodone, you can experience withdrawal.2
What Happens After You Quit Oxycodone?
How long do the withdrawal symptoms last once you quit oxycodone? The process usually unfolds in the following timeline:
- Days 1-2: Initial withdrawal: Symptoms usually start 8-12 hours after the last dose of oxycodone.
- Days 3-5: Intensified withdrawal: Symptoms are usually at their worse during this time. Muscle aches are common, along with shaking and cramps.
- Days 6-7: Psychological withdrawal: At this point, physical symptoms lessen, and psychological symptoms grow stronger. Depression and anxiety are common.
- Days 8 and beyond: Detoxed: After eight to 10 days, oxycodone has usually been purged from the body (detoxed). Physical symptoms are gone. However, psychological addiction may still be present. If this is the case, you should seek additional treatment.
Is it Safe to Stop Oxycodone Cold Turkey?
Because she ran out of pills, Lily abruptly stopped taking oxycodone. Quitting cold turkey like this can produce very distressing symptoms, both physical and emotional.
For people who have other health conditions, the body’s physical reaction can cause serious issues. Even in healthy individuals, severe vomiting and diarrhea can cause life-threatening dehydration. And many people start using the drug again in a desperate attempt to make the oxycodone withdrawal symptoms stop.
To prevent this unhealthy cycle, it is usually best to taper off oxycodone as part of a professional opioid addiction treatment program. This is what Lily decided to do.
What’s the Process of Weaning Off Oxycodone?
Lily consulted with her doctor to develop an oxycodone tapering plan that worked for her. This plan would slowly wean her off the drug, minimizing withdrawal symptoms and helping Lily adjust to daily life without oxycodone.
Tapering plans typically include the following important steps when weaning off oxycodone:1
- Flexible approach: The plan for tapering off oxycodone must consider the person’s risk, preferences, and goals.
- Initial decrease: The amount of the dosage decrease is less important than successfully achieving some form of initial decrease.
- Dose and interval: Tapering off oxycodone involves two separate processes: dose amount and the interval between doses. One or both can be adjusted throughout the weaning process.
- Slow progress: A slow taper is 5-10% dose reduction per month. This may be necessary if you’ve been using oxycodone for more than a year. A faster taper decreases doses by 10% per In extreme cases, where there is medical risk due to other conditions, a decrease of 30-50% may be appropriate. But this requires close monitoring.
- Scheduled dosing: If possible, it’s good to continue with the same dosing schedule. For example, if you’re used to taking prescribed oxycodone in the morning, continue to take it then.
- Pauses: Putting the tapering process on pause may be appropriate at some point in the process. This break gives you time to adjust to the new dosage and learn new coping skills.
- Progress: Tapering off oxycodone is considered a success as long as you’re making progress by reducing your oxycodone use.
- Support: During the weaning process, social support, mental health care, and physician supervision are important. Lily began seeing a counselor to help with her anxiety and depression.
- Healthy habits: Lily also benefited from developing ways to manage pain and maintain a healthier lifestyle. These included:
- Good sleep habits
- Healthy nutrition
- Physical activity
- Non-opioid pain medications
Medical Detox Helps You Successfully Quit Oxycodone
Sometimes, medications are used to help people detox from oxycodone. These FDA-approved treatments can help reduce oxycodone withdrawal symptoms and cravings. A healthcare provider prescribes the medication and closely monitors the patient’s progress. For some, this medical support can be the key for how to quit oxycodone.
Medical detox may involve one or more of the following medications:
- Buprenorphine: This is prescribed for moderate to severe oxycodone withdrawal. It reduces the person’s cravings for oxy and provides relief for withdrawal symptoms.3
- Methadone: This medication also reduces cravings and alleviates oxycodone withdrawal. It is used for medical detox from opioids that are longer acting, such as morphine.3
- Suboxone: This medication is a combination of buprenorphine and naloxone. It prevents cravings and blocks the intoxication effects of other opiates.4
- Other Medications: There are a number of drugs used during the detox process to treat withdrawal symptoms. Healthcare providers may prescribe medication to treat insomnia, nausea, diarrhea, and abdominal cramps. These may include temazepam, metoclopramide, and propantheline.3
Sources:
- Sarah.Rinn,. (n.d.). Tapering and discontinuing opioid use. Minnesota Opioid Guidelines. Retrieved November 29, 2023, from https://mn.gov/dhs/opip/opioid-guidelines/tapering-opioids/
- Doj/dea. (n.d.). Drugs of Abuse, A DEA resource guide (2020 edition). Retrieved November 30, 2023, from https://www.dea.gov/sites/default/files/2020-04/Drugs%20of%20Abuse%202020-Web%20Version-508%20compliant-4-24-20_0.pdf
- Withdrawal management. (2009, January 1). NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK310652/
- Grinspoon, P. (2018, March 20). 5 myths about using Suboxone to treat opiate addiction. Harvard Health. https://www.health.harvard.edu/blog/5-myths-about-using-suboxone-to-treat-opiate-addiction-2018032014496

Suboxone withdrawal is worse than heroin withdrawal.
No one has ever been able to successfully taper off Suboxone.
Tapering off Suboxone is something that’s shrouded in both mystery and myth. While the thought of stopping the medication certainly generates a bit of anxiety, the unknowns and “what ifs” are truly the drivers of fear. What will it feel like when your Suboxone dose is decreased? Will it feel like you’re in withdrawal 24/7? Will anyone help you if the taper is going too fast?
By answering the what ifs and shining a light on the unknowns, tapering off Suboxone suddenly becomes a lot less frightening. Once the fear is under control, you’re free to play a leading role in your own recovery process.
What is a Suboxone Taper?
 First thing’s first; let’s talk about what a Suboxone taper is and why it’s so important. Tapering is defined as gradually discontinuing or reducing the dose of a particular drug required by a patient over a prolonged period of time. Pay close attention to those last six words: “…over a prolonged period of time.”
First thing’s first; let’s talk about what a Suboxone taper is and why it’s so important. Tapering is defined as gradually discontinuing or reducing the dose of a particular drug required by a patient over a prolonged period of time. Pay close attention to those last six words: “…over a prolonged period of time.”
The process of tapering is, by definition, meant to be slow.
Suboxone is an FDA-approved medication that has changed the way opioid addiction is treated. Its unique combination of two distinctive chemical compounds – buprenorphine and naloxone – give it the ability to virtually eliminate opioid withdrawal symptoms and minimize the risk of abuse. It takes time to recover from opioid use disorders, so most patients take Suboxone for an extended period of time.
Since buprenorphine is a partial opioid agonist, it does carry a risk of dependency. Given this risk, when you’re ready to stop taking Suboxone, a supervised taper is always recommended.
Trying to quit “cold turkey” without assistance can be dangerous and cause painful withdrawal symptoms, both of which increase your odds of relapse. A supervised taper, on the other hand, significantly lowers or eliminates withdrawal symptoms and prepares your body for life beyond Suboxone.
What to Expect During a Suboxone Taper
The road to a successful Suboxone taper begins with open, honest dialogue between you and your clinician. From those conversations, you will work together to develop a plan to reduce the amount of Suboxone you take. The result is a tapering schedule that is highly individualized and focused on your personal needs instead of being focused on adherence to one specific approach.
Your dosage can be lowered a little bit at a time over several days, weeks, or even months. According to the National Alliance of Advocates for Buprenorphine Treatment (NAABT), Suboxone should generally be lowered in increments of 2 mg at a time every few days. Keep in mind, however, this progress relies on your level of dependence and individual experience. If you’re on a well-structured tapering schedule, you should only feel mild withdrawal symptoms for a few days following a reduction in dose.
If, at any point during the taper, your withdrawal symptoms or cravings become more intense, talk to your clinician. He or she can readjust your dose or slow the taper. You may need to go back to a previous dosage level in order to stabilize or increase the amount of time in between dosage reductions.
In some cases, a medication called Naltrexone may be used after you’ve tapered off Suboxone. Naltrexone is an opioid antagonist medication that works by blocking the effects of opioids. When used after the Suboxone tapering process, it offers additional anti-craving properties that can strengthen long-term sobriety. If used before the Suboxone taper is complete, however, Naltrexone can cause precipitated withdrawal.
Getting Help With Your Suboxone Taper
Some people might tell you that getting off Suboxone is impossible – that no one can handle the withdrawals or function without the medication. Thankfully, that isn’t true. With proper treatment and support, you can successfully taper off Suboxone.

Tracy was aiming for a vein, but she missed. Instead of entering her bloodstream, the heroin went directly into the fatty tissue around the vein. It hurt, but she figured it was no big deal.
She was wrong…
4 Dangers of Missing the Vein With IV Drug Use
 Injecting a drug (often called “shooting up”) means using a needle to deliver drugs like heroin, cocaine, and methamphetamine directly into a vein. When the needle fails to reach its target, this is called a “missed shot.”
Injecting a drug (often called “shooting up”) means using a needle to deliver drugs like heroin, cocaine, and methamphetamine directly into a vein. When the needle fails to reach its target, this is called a “missed shot.”
A “missed shot” happens when a needle either: 1) doesn’t enter the vein properly, 2) enters the vein then slips out again, or 3) enters the vein and goes all the way through to the opposite side of the vein.
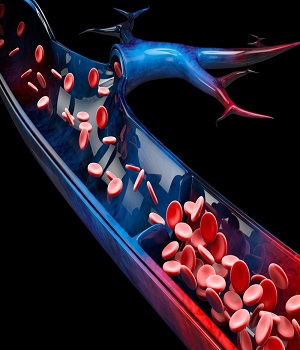
During IV drug use, when the needle slips or punctures the vein, it causes fluid to enter the tissue around the injection site. This often leads to infection, and from there, things can quickly go downhill. People can experience abscesses, cellulitis, vein collapse, and other complications.
Let’s take a look at four serious problems that can develop if IV drug users miss the vein.
#1 Abscesses
When a missed shot gets infected, you may get an abscess at the injection site. Your body is trying to fight the infection, so it sends cells to the damaged tissue to repair it. This causes the area to become swollen and fill with pus. (Pus is a mix of white blood cells that are sent to fight the infection, plus germs and dead tissue.)
Side effects of an abscess include:
- Redness of the skin
- Smooth swelling under the skin
- Pain in the infected area
- Warmth of the skin in that area
- A build-up of pus in the area
Because of the infection, you may also experience a fever and chills. Here’s how some people have described the abscess experience:
“It gets red, and it gets hot, and it hurts. It gets to a point when you just can’t bear it any more. You just can’t walk. Or you can’t use wherever it is on your body, you can’t use that limb. You can’t use your arm. You can’t use your leg or your foot. It becomes to where it’s like affecting you and you can’t function.” ~ 37-year-old woman
#2 Cellulitis
A missed shot can also lead to cellulitis. This is a deep, bacterial skin infection. It can occur when a break in the skin allows bacteria to invade (which happens when drugs are injected outside a vein). And it can be very serious.
Common symptoms of cellulitis include:
- Pain
- Tenderness
- Swollen skin
- Redness of the skin
- Bruising
- Blisters
- Fever
- Headache
- Weakness
- Chills
The pain and other symptoms start at the injection site, but the infection can spread quickly throughout the body. It can cause damage to tissue and tissue death. If you get cellulitis repeatedly, this can cause damage to your lymphatic drainage system and cause ongoing swelling of the affected arm or leg.
And the infection can enter your bloodstream, lymph nodes, bones, heart, or nervous system. At that point, it can become life-threatening. Complications from cellulitis can lead to amputation or even death. When you factor in the complications from addiction, it’s easy to see how things can spiral.
#3 Vein Collapse
Repeated missed shots can also cause your veins to collapse.
Here’s how it happens:
- The injection causes damage to the lining of the vein.
- Clots form around the damaged site.
- The clots harden into scar tissue.
- These clots narrow the vein, which restricts blood flow and causes future clots to form more quickly.
- Eventually, the sides of the vein heal together (the vein “collapses.). There’s so much scar tissue that it draws the sides together and shuts off the vein.
Once a vein collapses, blood can no longer flow through it. Sometimes a collapsed vein can heal, but the damage can be severe enough that the collapse is permanent. In some cases, this can cause circulation problems.
#4 Substance Complications
 In addition to the damage caused by the needle, the drugs themselves can irritate the vein or cause other issues. For example, research has shown that the acidity in heroin can damage veins. Researchers found that some batches of heroin have a pH level as low as 2.6 – which means the heroin is very acidic. (In comparison, lemon juice and vinegar both have a pH of 2.) Imagine the irritation your veins would experience with something that acidic flowing through them. With repeated exposure to such high pH levels, veins can develop life-threatening infections.
In addition to the damage caused by the needle, the drugs themselves can irritate the vein or cause other issues. For example, research has shown that the acidity in heroin can damage veins. Researchers found that some batches of heroin have a pH level as low as 2.6 – which means the heroin is very acidic. (In comparison, lemon juice and vinegar both have a pH of 2.) Imagine the irritation your veins would experience with something that acidic flowing through them. With repeated exposure to such high pH levels, veins can develop life-threatening infections.
It’s also worth mentioning that, when people inject heroin that is mixed with cocaine, the cocaine actually numbs the injection area. That means you aren’t able to feel the typical pain associated with missing the vein. And when you can’t feel it, you don’t know there’s a problem.
IV Drug Users Can Expect Complications
Are complications from missed shots a common problem? Are you likely to experience one of these issues? Well, over half (56%) of people who inject drugs admit they’ve missed a vein. And one in six intravenous drug users reports experiencing a missed shot more than four times every month.
So, yes, IV drug use problems are common, and the risks are high.
 How do we prevent opioid-related deaths?
How do we prevent opioid-related deaths?
Opioid-related overdose deaths continue to rise. But the public doesn’t want to deal with the problem in their city. Data from the Centers for Disease Control and Prevention show that overdose deaths rose nearly 30 percent in 2021.
The pandemic has only exacerbated the opioid crisis. And the crisis doesn’t have an end in sight, as newer, more potent opioids hit the street.
Public health officials are scrambling for solutions and agencies are increasing access to medication-assisted treatment. Communities are still largely opposed to methadone clinics in their town or city. This line of thinking is called “Not In My Neighborhood,” which is known by its acronym: NIMBY.
The only thing it’s doing is creating barriers to public health harm reduction efforts for the opioid epidemic.
Harm Reduction Helps Prevent Opioid-Related Deaths
 Harm reduction services like methadone clinics, safety syringe exchanges, and even safe consumption sites are resisted in almost every city.
Harm reduction services like methadone clinics, safety syringe exchanges, and even safe consumption sites are resisted in almost every city.
Sophia lives in New York City. She believes that the implementation of a safe consumption site is a disaster to the city.
“New York is already rife with addiction,” she says. “Bringing a ‘safe consumption site’ will only encourage addicts to swarm neighborhoods to use drugs, bringing crime, violence, and antisocial behavior to the city. I don’t want anything like that in my neighborhood!”
Those concerns are valid, and public safety concerns are important. However, Sophia does not get the full picture. However, medical professionals and researchers are working to shed light on the issue.
The Real Help of Harm Reduction
Dr. C. Debra M. Furr-Holden is an associate professor in the Bloomberg School of Public Health’s Department of Mental Health. She studies the effects of treatment centers on crime. Her Johns Hopkins Bloomberg School of Public Health research suggests there may actually be less serious crime near clinics than other community businesses. In fact, the research shows that drug treatment centers actually attract less crime than liquor stores and convenience stores.
Kathryn Stadeli is a surgical resident at the University of Washington. She is acutely aware of the effects of opioid-related overdoses in the state of Washington. She tells the Seattle Times that overdose-related deaths from fentanyl rose 70 percent in 2018 compared to the previous year.
Stadeli sees many of these deaths firsthand. She feels powerless over them.
“Unfortunately, opioid use disorder (commonly known as addiction) is not a disease I can cut away with a scalpel,” she says.
She suggests, however, that the use of certain medications can reduce the rate of opioid-related deaths by a staggering 50 percent. This method of treating opioid addiction is known as — known as medication-assisted treatment.
The problem: access.
Seattle, like many other cities, needs more medication-assisted treatment centers, like methadone clinics.
Stadeli talks about “Sarah,” whom she treated for a potentially deadly skin infection from injecting opioids. She explains that Sarah developed opioid use disorder after taking oxycodone for a sports injury. Like millions of other Americans who weren’t able to refill their prescription, Sarah turned to injecting heroin and fentanyl.
“I held her trembling hand as we wheeled her to the operating room; the fear invading her beautiful brown eyes when she asked me if she was going to die still haunts me,” Stadeli recalls.
Sarah had struggled to quit using on her own. Despite desperately wanting help, her situation and lack of housing meant that she wasn’t able to access the treatment she needed. Tragically, Sarah died from that infection shortly after her encounter with Stradeli.
“She was 22, and opioids killed her. Deaths like hers are preventable and unacceptable,” says the surgical resident.
The Benefits of Harm Reduction Services
Stadeli underscores the already substantial empirical evidence that that MAT is a far more successful treatment of opioid use disorder than alternatives, like rehab, resulting in less likelihood of overdoses. Those aren’t the only benefits.
The Substance Abuse and Mental Health Services Administration (SAMHSA) demonstrated that medication-assisted treatment:
- Improves patient survival
- Increases retention in treatment
- Decreases illicit opioid use and other criminal activities among people with substance use disorders
- Improves birth outcomes among pregnant women with substance use disorders
- Increases patients’ ability to gain and maintain employment
Yet, stereotypes about people who need medication, like methadone, persist. This stigma is a major barrier to treatment. This is why less than 10 percent of those with substance use disorder get the help they need.
In fact, research from the Recovery Research Institute shows that this stigma impacts the quality of care and how people with substance use disorders are treated.
Reducing Stigma to Prevent Opioid-Related Deaths
 Given that level of stigma, it’s understandable why folks don’t seek help. And trying to quit on their own is an uphill battle with low rates of success. Added to that stigma is the public perception of bringing medication-assisted treatment centers to their communities, like Sophia mentioned.
Given that level of stigma, it’s understandable why folks don’t seek help. And trying to quit on their own is an uphill battle with low rates of success. Added to that stigma is the public perception of bringing medication-assisted treatment centers to their communities, like Sophia mentioned.
Yet the evidence, like in Furr-Holden’s study shows the opposite to be true. Harm reduction facilities, like syringe exchange programs, methadone clinics, and other treatment facilities actually reduce the burden on the local economy by:
- Lowering rates of transmissible diseases, like HIV and hepatitis B and hepatitis C
- Reduce emergency department admissions
- Increased life expectancy and reduces overdose
- Improved access to treatment facilities and subsequently recovery
- Provided access to other critical services like housing and medical care
- Decreased the likelihood of engaging in criminal activities
- Reduced use of opioids
- Improved the likelihood of obtaining housing and employment
- Improves birth outcomes
Despite these overwhelmingly positive outcomes, being treated with methadone is still highly stigmatized. Most patients feel like they’re “dirty” for accessing this help.
How Can Destigmatizing Harm Reduction Services Prevent Opioid-Related Deaths?
Sarah Church, PhD, is the executive director of the division of substance abuse at the Albert Einstein College of Medicine. She mentions a quote from her colleagues, Murphy and Irwin, in a recent training:
After ten years of interviewing women and men in various stages of their methadone maintenance careers, recurring themes emerged, one of which was that being a methadone patient is a marginal identity; not quite junkie, not quite conventional. Clients’ efforts to manage this stigmatized identity were often shrouded in anguish and secrecy. Methadone patients were in a kind of identity limbo; a holding pattern between two extremely different social worlds. They were trying to affect an identity transformation; however, in many circumstances they were still associated with and defined by their ‘dirty secret.’
Prevent Deaths by Preventing NIMBY-ism
So, why we are still stigmatizing and resisting the very solutions to the opioid crisis because we don’t want it in our neighborhood?
Many would argue that, perhaps the solution to the opioid crisis isn’t only an increase in treatment facilities, particularly medication-assisted treatment facilities, but also the critical work of destigmatizing people with mental health disorders? What are your thoughts on the issue?
If you or someone you love is experiencing a substance use disorder, help is available. Call 800-934-1582(Sponsored) today.
 You may know him as a young John Conner in Terminator 3: Rise of the Machines. Or you may recognize him as the child actor who co-starred with Mel Gibson in Man Without a Face in 1993.
You may know him as a young John Conner in Terminator 3: Rise of the Machines. Or you may recognize him as the child actor who co-starred with Mel Gibson in Man Without a Face in 1993.
Nick Stahl began performing at age 4 and was recruited by Hollywood at age 10. He was just 11 when Gibson discovered Nick’s talent, and his career took off from there.
And it was just two years later, at age 13, that Stahl discovered alcohol.
But let’s back up a bit.
Looking back at his childhood, Stahl gains some insight into why the stage was so appealing – and why alcohol was so appealing at a young age, too.
A Blanket of Fear
 Stahl was raised by a single mom who worked two jobs to make ends meet.
Stahl was raised by a single mom who worked two jobs to make ends meet.
Stahl recalls, “From a very young age, I was always under this blanket of fear, financial fear. There was this idea that if we didn’t come up with enough money for that month, we would end up on the street. That colored my outlook growing up. My default mode was untrusting, with this mentality of waiting for the other shoe to drop.”
“I don’t look back on my childhood with real fond memories,” he says. “But for some reason, when I did plays, that stuff shut off and I had this ability to just be very comfortable.”
And when he had his first drink at 13, he discovered a way to “shut stuff off” when he wasn’t on stage. The tense feelings disappeared.
“Suddenly, I had a freedom from thinking, from uncomfortability,” he explains. “I felt okay in my skin — and I hadn’t really felt that before.”
Full Steam Ahead
By age 16, Stahl’s career was in full gear, and he and his mother moved to Los Angeles. There, he discovered the party scene.
He recalls, “I was going to bars. I had a very easy time getting into these places. A lot of my friends were older, and I had a great time.”
It wasn’t long before he was smoking weed. And from there, he moved on to pills, cocaine, and meth.
“That became what I chased,” he says. For Stahl, the drugs alleviated anxiety. He wasn’t partying for fun, but for release. He explains, “Very early on, it was not ‘I want this,’ but ‘I need this.’”
Falling Apart
In 2001, Stahl starred in Bully, a true-crime drama. Brad Renfro, his co-star, also battled addiction at the time.
Stahl recalls, “He was more severe in his addiction than I was. He just progressed to a point where he had to have someone on set with him to keep him sober.”
Stahl knew he was headed in the same direction. He tried to stop the deadly addiction train he was on.
“Throughout my 20s, I experimented with different ways to regulate my drinking. Maybe LA is the issue, right? So, I’d move. Maybe these certain friends I’m hanging out with, maybe that’s the issue. So, I’d get new friends.”
But none of that worked.
“Things started to get awful pretty quickly,” Stahl recalls. “I started to miss appointments. I put on a good front. The extent of my illness stayed hidden even from me. It’s common to justify, rationalize things. I looked around and said, ‘Everyone is partying the way I am.’ In retrospect, there were far less people going as hard as I did.”
In 2007, at age 27, Stahl entered rehab for the first time. In 2009, he tried again.
After two failed attempts at recovering from addiction in LA, Stahl moved back to his home state of Texas.
But Stahl couldn’t stay away from Hollywood for long. He went back – and was arrested multiple times. The charges included disorderly conduct and possession of meth.
Picking Up the Pieces in Recovering from Addiction
Despite his struggles, Stahl never lost an acting job. He was able to hold it together enough that he never got fired. But he knew he would soon, if something didn’t change. In 2012, he knew it was time to step away from acting for a while.
“I was physically there, but I was checked out,” he admits, “and I certainly wasn’t feeling any real enthusiasm for acting anymore. I knew that I had to step away, for self-preservation, but also for the preservation of my career, if I was going to have one again.”
Stahl spent the next five years in Dallas, “diving into his recovery” as he puts it.
“I didn’t think it would be easy, but it proved to be even more difficult than I thought it would be,” he says. “It’s hard to put my finger on what shifted. If I hit bumps in the road, I always got up and tried again. Luckily, I was resilient…One day, it just kind of stuck.”
Once he achieved sobriety, Stahl was able to give his life new direction. “It proved to be reconstructive for me,” he says. “That’s when I really started to piece together that I had neglected building a real life outside of the business. For many years, I had everything — but I didn’t have anything resembling a satisfying life. I didn’t have outside interests, I lost touch with friends and family. The film world made up too much of my identity.”
A New Life While Recovering from Addiction
When Stahl stepped away from Hollywood while recovering from addiction, he didn’t leave with millions in the bank. That meant he had to get a job like any other Joe. “So, I started working for a friend’s moving company,” he says.
 “I tried other things. I worked at a coffee shop in New York for a little bit. Not only did I learn how to live as a sober person, which I didn’t know how to do, but I learned how to have a life outside the business.”
“I tried other things. I worked at a coffee shop in New York for a little bit. Not only did I learn how to live as a sober person, which I didn’t know how to do, but I learned how to have a life outside the business.”
And this fresh perspective has allowed Stahl to re-enter show business with a healthy, sober outlook. “That passion inside me that burned for film and acting, it had dulled progressively over time,” he explains.
“But once I was separated from Hollywood, all of that started to come back. Over the past few years, whether I’m working on a film or auditioning, I don’t take it for granted, ever. I work much harder at it now. I just feel a renewed love for it.”
Clean for four years now, Stahl, age 41, is back in action with a full line-up of acting roles on his calendar.
But recovering from addiction comes first. “Recovery has to be the most important thing for me,” he says. “I put it first in my life. But I’m grateful for it, and it’s given me the opportunity to try to help people in the same situation I was [in]. It’s more important to me than making films. I search out people who have had similar struggles and show them how I got well. I speak from my experience and show them what worked for me.”
If you or someone you love is experiencing a substance use disorder, help is available. Call 800-934-1582(Sponsored) today.

80 members of Temple Sinai gathered for a Zoom call to hear their spiritual leader’s announcement.
They thought Rabbi Perice might have called the meeting to share that he and his wife were having a baby. Or that they were buying a home.
Or maybe that he was leaving his post.
Instead, he disclosed to his congregation that he’d been in recovery from opioid addiction for 10 years.
Perice explained that he shared this “because they trust me every day with the most vulnerable parts of their lives. What would it mean if I couldn’t trust them the way they trust me?”
Tearing Down the Stigma in Talking about Opioid Addiction
 “When the rabbi told me in advance what he wanted to say, I thought it was a great idea,” said Johanna Schoss, president of the Temple Sinai board.
“When the rabbi told me in advance what he wanted to say, I thought it was a great idea,” said Johanna Schoss, president of the Temple Sinai board.
“For someone like the leader of our community, for whom people already have a lot of respect, to admit to having gone through a situation like this, it means that other people don’t have to be afraid to talk about it.”
“Addiction is still something that is thought of as taboo, but if our rabbi and our community can help in any way, it’s huge,” said past board president Stacey Blacker.
With this support and encouragement from leadership, Perice moved forward with his announcement. And the positive response has been overwhelming.
“I was overwhelmed by the support that this community showed me,” Perice said. “I’ve heard from probably 50 people, sharing personal stories, congratulations, all the nice things you would hope to hear after sharing something like this.”
Perice hopes Temple Sinai can get involved in addiction and recovery efforts through education and advocacy–like talking about opioid addiction. He knows firsthand how important the right support can be.
A Fateful Collision
It started in 2007, with a simple car accident. Perice was rear-ended and suffered shoulder, neck, and lower back injuries. His doctor prescribed pain pills, which Perice took as directed – at first.
“It didn’t just seemingly fix the pain at first. I had been dealing with anxiety and depression, and [the drug] gave me almost a sense of peace. It took away the angst about college and jobs. And something in my brain said, ‘I need more of this.’”
Perice upped his dosage. But the physical pain worsened and his addiction grew. When his doctor refused to prescribe any more painkillers, he began doctor shopping. And that’s when his life began to revolve around fending off withdrawal.
“I told myself, ‘I can’t be an addict,’” he said. “I was getting it from a doctor. I had legitimate pain. How can I be an addict? But after two years went by, doctors were no longer close to prescribing what I needed.”
“I needed to find other ways — calling friends and acquaintances, going into medicine cabinets and checking wherever I could get it. That’s when I was introduced to OxyContin, which is a very powerful opiate. That was the medication I was most actively using until the end.”
A Fateful Moment of Clarity in Talking about Opioid Addiction
In 2011, Perice’s life took a turn. One day in early spring, he ran out of OxyContin. He couldn’t find anyone who had the drug.
He was desperate to relieve his withdrawal. So, he called a known drug source and told him “I need something, anything.”
An hour later, the man brought Perice a bag of heroin.
Perice had never done heroin before. He sat in his bathroom, staring at the bag.
“It was a moment I can only describe as a moment of clarity. I was able to see that if I did this, I might die. I just flushed it down the toilet, called my parents, and said, ‘I need help.’”
He got treatment, which included a long-term medically assisted outpatient treatment, counseling, and physical therapy.
A New Path
Perice admitted, “Treatment saved me, but it didn’t give my life purpose. Re-finding my faith gave me purpose.”
 Once he was “liberated from opioids” as he put it, Perice began considering the rabbinate. He entered Reconstructionist Rabbinical College in 2014 and was ordained in 2020.
Once he was “liberated from opioids” as he put it, Perice began considering the rabbinate. He entered Reconstructionist Rabbinical College in 2014 and was ordained in 2020.
He became the religious leader at Temple Sinai within a month of ordination.
After serving there for several months, Perice decided to share his secret with his congregation. And he’s glad he did. He described it as “a very powerful moment for me, and for my community.”
He added:
“But there are a lot of feelings about the issue [of addiction] in the world. Many people have dealt with this in their families. Addiction causes pain for everyone around [the person living in addiction].”
“So, it’s important to help people move through that pain. By removing the stigma and getting people help early, we can help them, and their families, heal.”
If you or someone you love is experiencing a substance use disorder, help is available. Call 800-934-1582(Sponsored) today.

10.1 million. That’s the estimated number of Americans aged 12 or older who misused opioids in 2019.
There were an estimated 75,673 opioid overdose deaths that occurred from April 2020 through April 2021.
What are we doing about these alarming statistics? The FDA has approved three drugs to treat opioid dependence. Buprenorphine – sold under the brand name Suboxone – is one of them.
Here’s how it works and what researchers have discovered.
Suboxone 101
 Suboxone is an opioid partial agonist. An agonist is a chemical that triggers a response in the body. This drug only partly activates rather than fully. So its effects are weaker than substances like heroin or morphine (which are full agonists).
Suboxone is an opioid partial agonist. An agonist is a chemical that triggers a response in the body. This drug only partly activates rather than fully. So its effects are weaker than substances like heroin or morphine (which are full agonists).
The drug also has a ceiling effect. This means higher doses don’t increase its effects. And, it’s long-acting, so people don’t have to take it every day.
This makes Suboxone a go-to drug for medication-assisted treatment (MAT) for opioid use disorder.
This medication can:
- Diminish the effects of physical dependency on opioids, such as withdrawal symptoms and cravings
- Increase safety (reduce the chances of overdose)
- Lower the potential for drug abuse
Ultimately, this can help people withdraw from opioids like heroin and reduce people’s use.
If it is taken as prescribed, buprenorphine is reported to be safe and effective.
How long someone takes buprenorphine varies with each case. Treatment can range from short-term to indefinite.
MAT 101
The US Department of Health and Human Services reports that 1.27 million Americans are now receiving medication-assisted treatment for opioid use disorder (OUD). This combines medication like buprenorphine with counseling and behavioral therapies. This creates a comprehensive treatment plan that treats the whole person.
Research has shown that this combination can successfully treat opioid use disorders and help sustain recovery.
SAMSHA states the ultimate goal of MAT is “full recovery, including the ability to live a self-directed life.”
Does It Work?
Researchers recently dug into results from drug tests to find out.
Brendan Saloner, PhD, is an associate professor at Johns Hopkins Bloomberg School of Public Health. Together with researchers from Millennium Health, he published their findings in JAMA Network Open.
These investigators analyzed 150,000 urine drug test results for OUD patients. The patients were prescribed Suboxone between 2013 and 2019. Researchers wanted to find out if the presence of Suboxone made it less likely for a person to misuse opioids.
Of their 150,000 results, 85.49 percent were positive for buprenorphine. Just under half (47.58 percent) were positive for at least one non-prescribed substance.
They discovered that patients who tested negative for prescribed buprenorphine “were significantly more likely” to test positive for other substances, compared to those who tested positive for buprenorphine.
Specifically, they found:
- Those who tested negative for buprenorphine were 10 times more likely to test positive for heroin.
- Those who tested negative for buprenorphine were seven times more likely to test positive for fentanyl.
In other words, the results indicate that if the patients stuck with their treatment, they were less likely to abuse other drugs. And, that if they stopped taking their medication, they were much more likely to turn to other drugs.
More Good News for Suboxone

Credit: Kzenon, Rido, Syda Productions, Victoria Ashman, Rawpixel.com, fizkes, Dragon Images, Simone Hogan
Other research supports the theory that Suboxone can be an effective treatment for addiction. One meta-analysis of buprenorphine use found that doses of this medication improved retention in treatment and that high doses reduced opioid use.
And through other research, MAT has been shown to:
- Increase treatment retention
- Increase patients’ ability to remain employed
- Decrease illicit opioid use and other criminal activity among those with SUDs
- Improve patient survival
Call 800-934-1582(Sponsored) to learn more about available treatment options near you.

You say tomato. I say tomahto.
You say oxycodone. I say Percocet. Same difference, right?
Actually, no. The two drugs do have some similarities, but when comparing opioids, the terms are not interchangeable.
Let’s talk about how they differ.
Chemical Makeup
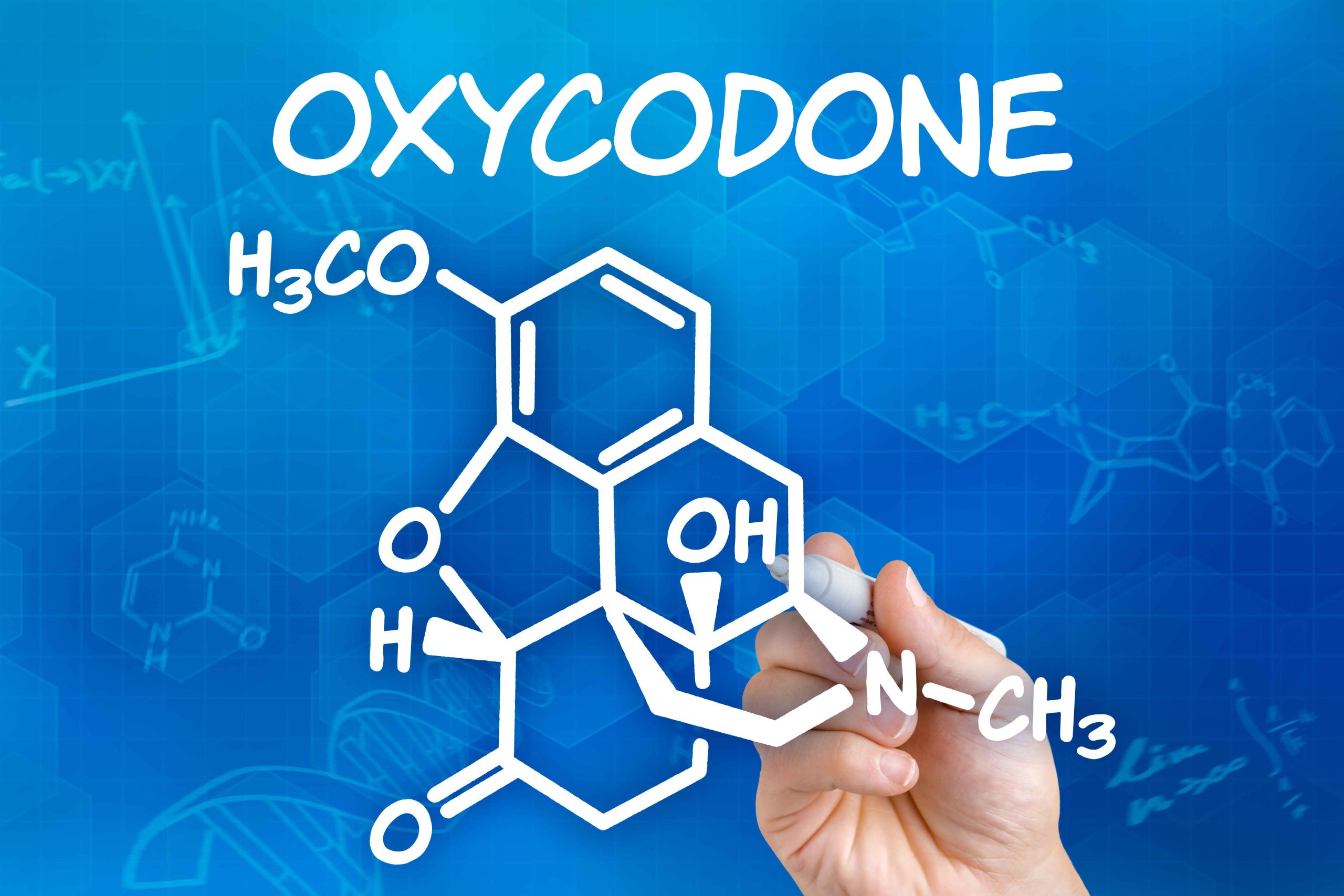
 Both of these drugs are opioid pain medications. Oxycodone is a synthetic drug made from opium. Percocet is made of oxycodone and acetaminophen. (Acetaminophen is another painkiller, which you probably know by its brand name: Tylenol.)
Both of these drugs are opioid pain medications. Oxycodone is a synthetic drug made from opium. Percocet is made of oxycodone and acetaminophen. (Acetaminophen is another painkiller, which you probably know by its brand name: Tylenol.)
If you take either of these drugs, you’re taking oxycodone. But when you take Percocet, you’re also getting the second medication, acetaminophen. This is one of the primary reasons oxycodone and Percocet get confused when comparing opioids.
Oxycodone is a generic drug, which is sold under several brand names. Percocet is one if the brand name drugs made with oxycodone.
Oxycodone and Percocet Use
Oxycodone is available in three different forms, which are used for different types of treatment:
- Immediate-release tablets enter the bloodstream right away
- Extended-release tablets gradually release the drug into the bloodstream
- An oral solution, often given through a gastric tube, is available for patients who can’t swallow tablets
Oxycodone is used for treating moderate to severe pain. The extended-release form is often prescribed for patients who have ongoing pain, such as cancer-related issues.
Percocet is also prescribed to treat moderate to severe pain. But it is used for treating conditions that also cause a fever because acetaminophen is a fever reducer. It may also be used to treat patients who experience pain while on another long-acting painkiller.
Percocet is not recommended for long-term use, since the acetaminophen in it can wreak havoc on the liver and cause serious damage over time.
Effectiveness
Both drugs are proven to effectively relieve pain. When you take Percocet or immediate-release oxycodone, you start to feel relief within half an hour, and the effects usually last for three to six hours.
Extended-release oxycodone starts to work within two hours and continues to relieve pain for up to 12 hours. The brand name drug OxyContin is a type of extended-release oxycodone.
Over time, patients can develop tolerance to these drugs. This means they need higher doses to get the same pain relief. Tolerance can begin to develop within just one week of taking regular doses of either drug.
Side Effects
Since we’re comparing opioids with the same primary ingredient, both oxycodone and Percocet naturally have similar side effects.
Both commonly cause:
- Constipation
- Sleepiness
- Calmness
- Nausea
- Dizziness
- Loss of appetite
- Headache
- Impaired motor skills
There are two main differences in their side effects:
- Oxycodone is more likely to cause feelings of euphoria
- Percocet can cause abdominal pain, black stools, and yellowing of the skin (jaundice) because of its effect on the liver
One of the biggest potential side effects of either drug is addiction. Tolerance can happen quickly and lead to physical and psychological dependence, so “>both drugs are considered highly addictive.
Drug Classification
Here’s an area where the two drugs don’t differ. The Drug Enforcement Administration (DEA) classifies drugs into five categories or “schedules.” A drug’s class is determined by its potential for dependency and its accepted medical use.
Both oxycodone and Percocet are Schedule II drugs.
Schedule II substances have “a high potential for abuse, with use potentially leading to severe psychological or physical dependence.” They are considered dangerous.
Other examples of Schedule II drugs include methamphetamine, cocaine, fentanyl, and Ritalin.
Pop Quiz
 Here’s a quick quiz comparing oxycodone and Percocet. Don’t worry – you won’t be graded!
Here’s a quick quiz comparing oxycodone and Percocet. Don’t worry – you won’t be graded!
Match the following descriptions with the correct drug. (Hint: Some are true for both substances.)
- An opioid
- Contains acetaminophen
- Relieves pain
- Is considered addictive
- Comes in an extended-release form
- Can cause drowsiness
- Reduces fever
- Is not recommended for long-term use
- Tolerance can develop in 7 days
- A Schedule II narcotic
How’d you do? You can check your answers below.
And remember, if you’re trying to decide which medication is best for your situation, always consult with a doctor and use the drug only as prescribed.
If you need help with drug abuse, call 800-934-1582(Sponsored) .
Pop Quiz Answers:
- Both
- Percocet
- Both
- Both
- Oxycodone
- Both
- Percocet
- Percocet
- Both
- Both
 Tina and Melinda are both addicted to opioids. Both of these women are paying for suboxone treatment for their opioid use disorder.
Tina and Melinda are both addicted to opioids. Both of these women are paying for suboxone treatment for their opioid use disorder.
Tina has private insurance. Melinda has Medicaid coverage.
Which of these two women is more likely to get an appointment? Will providers discriminate when it comes to the method for paying for suboxone treatment?
That’s what researchers wanted to find out. So, they used “secret shoppers” to get answers.
Investigators from Baylor University’s Hankamer School of Business, RAND Corporation, and Vanderbilt University Medical Center’s Departments of Pediatrics and Health Policy collaborated on the study.
Here’s what they discovered.
It’s Hard for Anyone to Get an Appointment
 Researchers made 3,420 simulated patient calls for the study. The callers identified themselves as women with Medicaid coverage or private insurance coverage. All were requesting appointments with buprenorphine providers.
Researchers made 3,420 simulated patient calls for the study. The callers identified themselves as women with Medicaid coverage or private insurance coverage. All were requesting appointments with buprenorphine providers.
Guess how many successfully landed an insurance-covered appointment? Less than half. Even with Medicaid or private insurance.
Only 45 percent of women with private insurance coverage were able to get an appointment. And just 38 percent of women with Medicaid insurance were as well.
According to the study’s lead author Michael Richards, MD, PhD, MPH, and associate professor at Baylor University in Waco:
The most striking finding is — for both callers that had private insurance and callers that had Medicaid — just how infrequently they’re able to actually leverage those insurance benefits when it comes to getting an appointment for opioid use disorder. That really speaks to the many serious and substantive access hurdles these individuals have to clear.
It’s Harder for Medicaid Patients…in Certain Areas
Previous research has shown significant differences in access to opioid use disorder treatment between patients with Medicaid versus private insurance. And this study was no different.
However, researchers discovered that these results varied based on one key factor.
Researchers found that callers with Medicaid were 11 percent less likely to get an appointment if Medicaid coverage was not common in the surrounding community.
But, as the percentage of Medicaid coverage in the local community went up, so did the number of Medicaid patients getting appointments.
In areas where Medicaid coverage was prevalent enough, the difference in access to care was insignificant.
Causes of Discrimination in Paying for Suboxone Treatment
Investigators can’t say for sure what is causing this disparity. They suspect it might be as simple as paperwork issues.
According to the study findings, providers in areas with a higher rate of Medicaid coverage may be more familiar with business processes needed to obtain payment from Medicaid for buprenorphine treatment.
But the problem is most likely multifaceted, they admit.
Whatever the issues are, researchers suggest that these findings guide future efforts. They advise, “Efforts to improve access to treatment may be best targeted to areas where Medicaid prevalence is lower.”
MAT Numbers Remain Low
 In 2020, nearly 70,000 people in the United States died from opioid overdoses. Currently, buprenorphine is one of three medication-assisted treatments (MAT) approved by the World Health Organization and the FDA to treat opioid use disorder. This medication can help diminish withdrawal symptoms and cravings.
In 2020, nearly 70,000 people in the United States died from opioid overdoses. Currently, buprenorphine is one of three medication-assisted treatments (MAT) approved by the World Health Organization and the FDA to treat opioid use disorder. This medication can help diminish withdrawal symptoms and cravings.
This, in turn, lowers the potential for opioid misuse.
The number of clinicians who can prescribe buprenorphine has increased 300 percent. But less than 33 percent of individuals with opioid use disorder receive any kind of MAT. Researchers hope their efforts can make a change in these numbers.
“Making it through the structural barriers to just getting into treatment for opioid use disorder is extraordinarily hard, even if you’re the most motivated person on the planet,” says study principal investigator Stephen Patrick, MD, MPH. He’s from the department of health policy at Vanderbilt University Medical Center in Nashville, Tennessee.
“We are seeing record-setting rates of overdose death, and for every overdose death, there are a slew of other hospitalizations and additional family members affected. I hope our continued research garners the attention of the public and policymakers and more clearly communicates that we must put solutions in place to break down these barriers.”
Call 800-934-1582(Sponsored) now to learn more about the available treatment options in your area.
 Over 93,000 Americans died from an opioid overdose in 2020, which is a 30 percent increase from the previous year. The effects of fentanyl are the root cause behind this increase. It is a powerful synthetic opioid that is infiltrating the drug supply.
Over 93,000 Americans died from an opioid overdose in 2020, which is a 30 percent increase from the previous year. The effects of fentanyl are the root cause behind this increase. It is a powerful synthetic opioid that is infiltrating the drug supply.
Americans are buying other drugs, like cocaine or benzodiazepines, that have been laced with fentanyl. Because the effects of fentanyl are so powerful, it is killing record numbers of unsuspecting Americans.
Fentanyl is not only potent but also difficult to identify. Given the social restrictions and heightened stress during the pandemic, more and more people had been susceptible to this deadly drug.
In this blog, we’ll explain why fentanyl is so dangerous, how to spot it in your drugs, and what to do if you suspect someone is having an opioid-related overdose.
What Is Fentanyl?
Fentanyl is a powerful synthetic opioid that is 50 times stronger than heroin and 100 times stronger than morphine. It has been used medicinally to treat chronic pain following surgery or in patients with cancer since 1968. Fentanyl is also illicitly manufactured for the drug market for those seeking a more powerful high than heroin.
Street fentanyl is either injected in its liquid form, smoked, or inhaled. Street names for fentanyl include:
- Murder 8
- Apache
- Dance Fever
- Jackpot
- Friend
- Goodfellas
- Tango and Cash
The typical effects of fentanyl are similar to heroin, and include:
- Euphoria
- Relaxation
- Pain relief
- Sedation
- Confusion
- Nausea and/or vomiting
- Dizziness
- Drowsiness
- Pupil constriction
- Risk of overdose and death
There is another contributing factor to the rise in fentanyl use. Drug manufacturers are cutting other drugs with fentanyl to cut down on costs while making the laced drugs more powerful and addictive.
What Does Fentanyl Look Like?
Prescription fentanyl is usually a patch worn on the skin. Illicitly manufactured fentanyl is available in a powder or liquid form. The powder is either white, gray, or tan-colored.
Unfortunately, when fentanyl is powdered, it’s difficult to differentiate it from other powdered drugs, like cocaine. And the liquid can be hidden in unassuming everyday items like nasal sprays, eye drops, and even candy.
Why Is Fentanyl So Dangerous?
According to the CDC, fentanyl and other synthetic opioids are the most common drugs involved in overdose deaths.
The CDC reports that over 150 people die from opioid overdoses from synthetic opioids like fentanyl every day.
The problem with fentanyl is two-fold: Its potency and the incentive of illicit drug manufacturers to cut other drugs with fentanyl to make more money.
People are buying illicit drugs like methamphetamine, cocaine, heroin, and pills (like opioids and benzodiazepines) completely unaware that their drugs are contaminated with fentanyl. What’s more, the amount of fentanyl in the drug could be a lethal dose that you can’t taste, smell, or see.
To make matters worse, rates of fentanyl infiltrating the drug supply continue to rise.
According to the Office of National Drug Control Policy, the rate of fentanyl-related overdoses has risen six-fold since 2014.
Fentanyl was involved in a staggering 62 percent of opioid deaths in 2020. Illicit manufacturers have been able to achieve exponential distribution across the country.
Previously, fentanyl was common in the northeast, midwest, and mid-Atlantic and now it is showing up in other parts of the country.
Why Did Overdose Deaths Surge During the Pandemic?
Fentanyl-related deaths have also been exacerbated by the pandemic. People struggled to access harm reduction programs that enabled them to test their drugs and access recovery resources.
This led many to return to using to cope with the stress, anxiety, and social isolation of the pandemic.
While the pandemic is beginning to wane, many people are burned out and struggling to cope with the economic burdens and the loss of loved ones that the pandemic left in its wake. These factors alone are a risk for overdose but taken together, they reflect one of the many tragedies of COVID-19 — the staggering rise of overdose deaths.
How Much Fentanyl Is Fatal?
It takes just two milligrams of fentanyl to kill, according to the Drug Enforcement Administration (DEA). You may think you’re safe because you don’t take opioids, but you’d be mistaken.
In recent seizures, the DEA found that 42 percent of counterfeit pills contain 0.2 to 5.1 milligrams of fentanyl.
Fentanyl is usually distributed by drug organizations by the kilogram. This amount could kill a staggering 500,000 Americans.
What Are the Signs of an Overdose?
Whether you’re taking a prescribed opioid, or an illicit substance, you should be aware of the signs of overdose because you could save someone’s life.
The common signs of overdose the CDC advises to look out for include:
- Shallow, weak, or no breathing
- Small pinpoint pupils
- Falling asleep or losing consciousness
- Limp body
- Choking or gurgling sounds
- Cold and/or clammy skin
- Discolored skin, especially on the lips and nails
What to Do If You Think Someone Is Overdosing
If you suspect someone is overdosing you should act quickly, by:
- Calling 911 immediately
- Administering the overdose reversal drug, naloxone
- Try to keep the person awake and breaking
- Lay the person on their side to prevent choking
- Stay with the person until the emergency services arrive
Naloxone (or brand name Narcan) is available in all 50 states. It is available from most pharmacies without a prescription. You can also get it for free from many recovery centers, outreach, and harm reduction programs.
It is very simple to use and will save a life.
How Can I Check My Drugs for Fentanyl?
It is possible to test your drugs for fentanyl and other potent opioids like carfentanil by using fentanyl test strips. You can either buy or find it at your nearest harm reduction service center. The test takes just 5 minutes and could save you from the harmful effects of fentanyl.
Fentanyl Myths
On TV dramas, cops come out in hazmat suits because they fear they’ll die from touching fentanyl. However, much of the media has misrepresented what happens when you come into contact with fentanyl.
The Harm Reduction Coalition has dispelled many of these myths, such as:
- You cannot overdose by simply touching powdered fentanyl. It must either enter your bloodstream or mucus membrane — body cavities like the nose, mouth, lungs, and stomach — for you to feel any of the effects of fentanyl.
- Fentanyl and its analogues, such as carfentanil, are not resistant to naloxone. Fentanyl is an opioid and therefore naloxone will respond to a fentanyl-related overdose. When people don’t respond to naloxone, it is because you haven’t waited long enough. (Fact: You need to wait two to three minutes. After, if still unresponsive, the person needs more than one dose).
- Fentanyl patches are not the same formulation as illicitly manufactured fentanyl. They are specially formulated for pain management — it takes 12 to 24 hours to receive adequate pain relief.
Ways to Reduce the Risk of Overdose from the Effects of Fentanyl
 While treatment is the preferred course of action for addiction, you may not be ready for recovery. Or, you may be concerned for a loved one who uses alone.
While treatment is the preferred course of action for addiction, you may not be ready for recovery. Or, you may be concerned for a loved one who uses alone.
This is where harm reduction practices apply. The following precautions can reduce the risk of overdose:
- Always carry naloxone
- Eat, drink, rest, and hydrate as best you can
- Make an overdose plan with a friend
- Use less and more slowly because fentanyl is very powerful
- Test your drugs
- Use one drug at a time
- Avoid taking alcohol with opioids
- If you do use alone, ensure someone knows where you are
- Be cautious of your tolerance, especially if you have recently taken a break from drug use. If in doubt, try a tester amount
- Use a different method of ingestion, such as snorting instead of injecting
If you or someone you love is experiencing a substance use disorder, help is available. Call 800-934-1582(Sponsored) today.
